Measles for Medical Professionals
03/18/2024 - Centers for Disease Control and Prevention (CDC) Health Alert Network (HAN) Health Advisory
Public Health Measles Updates
-
As of 03/18/2024, the CDC issued a Health Alert Network (HAN) Health Advisory to inform clinicians and public health officials of an increase in global and U.S. measles cases and to provide guidance on measles prevention for all international travelers aged ≥6 months and all children aged ≥12 months who do not plan to travel internationally. Follow the link to view the CDC HAN Health Advisory PDF.
-
As of May 18, 2024, there have been 8 confirmed cases of measles reported in California in 2024.
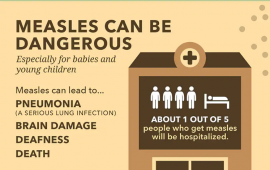
Measles clinical features
Measles is an acute viral respiratory illness. It is characterized by a prodrome of fever (as high as 105°F) and malaise, cough, coryza, and conjunctivitis -the three “C”s -, a pathognomonic enanthema (Koplik spots) followed by a maculopapular rash. The rash usually appears about 14 days after a person is exposed. The rash usually spreads from the head to the trunk to the lower extremities. Patients are considered to be contagious from 4 days before to 4 days after the rash appears. Of note, sometimes immunocompromised patients do not develop the rash.
When to suspect measles
Healthcare providers should consider measles in patients with:
-
Fever, rash, and any of the “3 Cs” – cough, coryza (runny nose), or conjunctivitis
-
In the prior 3 weeks, any: travel outside of North America, transit through U.S. international airports, or interaction with international visitors (including at U.S. tourist attractions).
Ask about measles vaccination status, onset and duration of fever and rash, exposure to other persons with febrile rash illness, travel history, and international visitors in the three weeks prior to illness. When suspecting measles in your patient, immediately mask and isolate the patient per airborne precautions. Infected people are contagious from 4 days before rash onset through 4 days after rash onset.
Recommendations for suspected cases of measles
-
Mask the patient immediately. If an infant or young child cannot wear a surgical mask, use another practical means of source containment during escort to an isolation room, such as placing a blanket loosely over the head (to not restrict breathing).
-
Bypass the waiting room if possible: keep patients out of the waiting area or other common areas.
-
Isolate the patient immediately, in an airborne infection isolation room (AIIR) if possible. See CDC and CDPH (PDF) infection control guidance. Infected people are contagious from 4 days before rash onset through 4 days after rash onset.
-
All healthcare personnel entering the patient room, regardless of immune status, should use respiratory protection at least as effective as an N95 respirator per Cal/OSHA requirements.
-
Promptly telephone the Shasta County Public Health to report suspected measles cases, even before laboratory confirmation. Call (530) 225-5591 | After Hours: (530) 339-9940
-
If advised to test for measles by your LHD, submit a specimen for measles polymerase chain reaction (PCR) testing. (Measles IgM testing is frequently falsely positive and is not recommended).
Ensure that patients are up to date on measles vaccinations. Before traveling abroad:
-
Infants 6 to 11 months old need 1 dose of MMR vaccine.
-
Children 12 months and older need 2 doses of MMR vaccine.
-
Adults born during or after 1957 without evidence of immunity against measles need documentation of two doses of MMR vaccine at least 28 days apart.
MMR Vaccination
Measles can be prevented with measles-containing vaccine, which is primarily administered as the combination measles-mumps-rubella (MMR) vaccine. The combination measles-mumps-rubella-varicella (MMRV) vaccine can be used for children aged 12 months through 12 years for protection against measles, mumps, rubella and varicella. Single-antigen measles vaccine is not available.
One dose of MMR vaccine is approximately 93% effective at preventing measles; two doses are approximately 97% effective. Almost everyone who does not respond to the measles component of the first dose of MMR vaccine at age 12 months or older will respond to the second dose. Therefore, the second dose of MMR is administered to address primary vaccine failure [1]
Clinical tools and resources
-
For Healthcare Professionals - Diagnosing and Treating Measles (CDC)
-
Measles Information and Data California Department of Public Health (CDPH)
-
Should I Test For Measles? A Guide for California Healthcare Providers (CDPH)
-
Measles Healthcare Exposure Investigation Quicksheet (CDPH)
-
Immune Globulin for Measles Post Exposure Prophylaxis (CDPH)
-
Report a Communicable Disease (Shasta County Public Health)
Information for patients
-
Measles Information (CDC)
-
Measles Information and Data (CDPH)
-
Immunization Information (Shasta Shots)
Updated May 16, 2024 | Public Health Communicable Disease Unit
Content source: Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases, Division of Viral Diseases, California Department of Public Health